Temperature regulation
Describe how body temperature is regulated
Define the interthreshold range of body temperature and the thermoneutral zone and provide the normal values
Core body temperature
- the temperature of the body's deep tissues and organs
- maintained by hypothalamus at 37 +/- 0.5C
Interthreshold range
- the range of core body temperatures when thermoregulatory responses do not occur
- 37 +/- 0.2°C in normal adult (i.e. 0.4°C)
- 37 +/- 2°C in anaesthetised adult (i.e. 4°C)
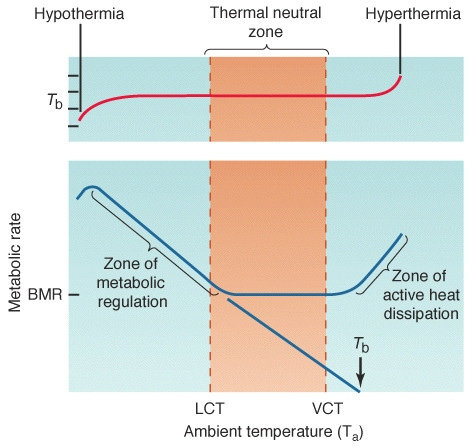
Thermoneutral zone (TNZ)
- the range of environmental temperatures where core body temperature is maintained by vasomotor activity without a significant change in metabolic rate
- i.e. there is no active heat production (shivering, non-shivering thermogenesis) or active heat dissipation (sweating, behavioual response)
- 27-31°C in a naked adult, lower if clothed
From Solar radiation by Amy L. Norris and Thomas H. Kunz, licensed under CC-BY 3.0
Explain how the body detects and defends against cold (or heat) exposure
Sensation of temperature (thermoception)
Peripheral thermoreceptors
- Located in skin and detect peripheral body temperature
- Cold receptors (Krause corpuscle) → detect cold, predominantly by Aδ fibres
- Warm receptors (Ruffini corpuscle) → detect warmth, predominantly by C fibres
- Signals ascend to the hypothalamus in the lateral spinothalamic tract
Core thermoreceptors
- Located in the spinal cord, abdominal viscera and great veins
- Detect core body temperature
- Referred to in some texts as central thermoreceptors
- Contain both cold- and warm-sensitive receptors
Central thermoreceptors
- Located in the anterior hypothalamus (preoptic area)
- Detect the temperature of local tissue and blood
- Contains cold- and warm-sensitive neurones
- Cold-sensitive neurons → increased firing with cooling
- Warm-sensitive neurons → increased firing with warming
Neural integration of temperature signals
All thermal inputs (including from the anterior hypothalamus) are integrated in the posterior hypothalamus, which determines the temperature set point and interthreshold range.
Temperature set point
- The posterior hypothalamus determines the temperature 'set point' around which body temperature is regulated
- The set point increases in response to pyrogens, particularly interleukin-1 (IL-1), which mediate fever
- The set point is also influenced by:
- Diurnal variation - lowest in the early morning, highest in the evening
- Menstrual cycle - higher in the luteal (second) half of the cycle
Interthreshold range
- The posterior hypothalamus determines the interthreshold range.
- The interthreshold range also varies with other hypothalamic influences, including:
- Thyroid hormones (T3/T4)
- Circadian rhythm
- sedation
Effector pathways
Thermoregulatory responses engage when body temperature is outside of the interthreshold range. Further deviation of temperature beyond the thermoneutral zone triggers additional thermoregulatory responses, which require an increase in basal metabolic rate.
Response to low body temperature:
- Below the interthreshold range:
- cutaneous vasoconstriction
- minimises heat loss to the environment by convection
- to a lesser degree, there is decreased radiant and conductive heat loss
- mediated by noradrenaline release through the sympathetic nervous system (SNS)
- heat-seeking behaviour
- cutaneous vasoconstriction
- Below the thermoneutral zone:
- piloerection (goosebumps) - traps warm air at the skin
- mediated by acetylcholine (ACh) release through the SNS, activating arrector pili muscles
- the skin is the only place in the SNS where post-ganglionic fibres release ACh
- thermogenesis
- piloerection (goosebumps) - traps warm air at the skin
Piloerection via activation of arrector pili muscles.
(1) epidermis, (2) arrector pili, (3) hair, (4) dermis.
By Anthony Caccese, licensed under CC-BY-SA 4.0
Response to increased body temperature:
- Above the interthreshold range:
- cutaneous vasodilation
- via inhibition of SNS afferents affecting cutaneous blood flow
- increases heat dissipiation by convection
- behaviour seeking a cooler environment
- cutaneous vasodilation
- Above the thermoneutral zone:
- sweating
- eccrine sweat glands in the dermis are activated, secreating sweat through pores in the skin
- mediated by ACh release through the SNS
- by increasing the rate of sweat production, there is less time for Na reabsorption within the eccrine duct
- → less water reabsorption → more sweat secretion
- ↑ evaporative heat loss
- apocrine sweat glands are minimally involved in thermoregulation
- eccrine sweat glands in the dermis are activated, secreating sweat through pores in the skin
- sweating
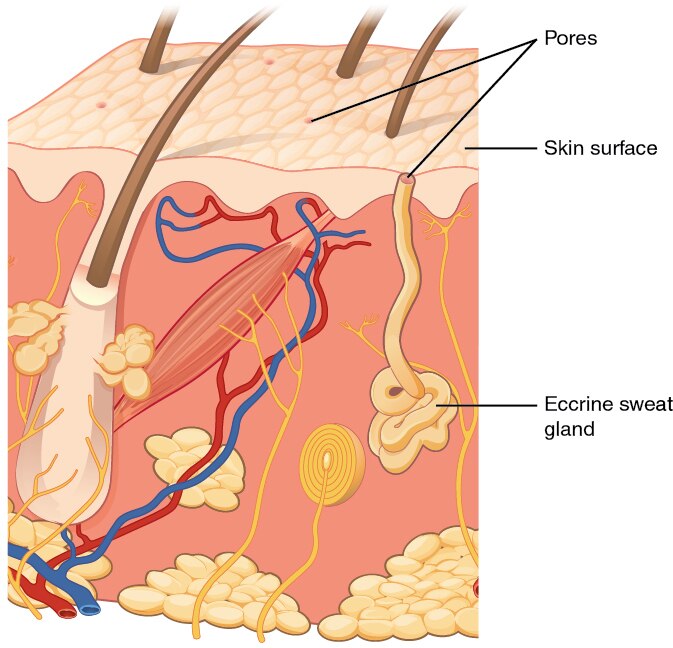
Sweat secretion by eccrine glands increases with body temperature.
By OpenStax, licensed under CC-BY-SA 4.0
Thermogenesis
The body generates heat by increasing metabolic activity through various mechanisms.
-
Voluntary muscle activity
- e.g. moving on the spot when you are cold
-
Involuntary mechanisms work by increasing basal metabolic rate (BMR) and kick in below the thermoneutral zone
- shivering
- non-shivering thermogenesis
- endocrine response
- hunger
Shivering
Rapid, oscillatory muscle activity that greatly increases heat production.
Comprised of
- cyclical contractions up to 250Hz - likely peripherally mediated
- superimposed slow synchronised waves - likely centrally mediated
- rigors appear when shivering is more intense (10-20Hz)
Shivering can increase BMR by 100% in adults.
Non-shivering thermogenesis
Mediated by beta3 receptors in brown adipose tissue and skeletal muscle.
Mechanism
- brown fat has rich vascular supply and adrenergic innervation with abundant mitochondria
- lipolysis liberates substrates for the electron transport chain (ETC)
- oxidative phosphorylation is uncoupled
- energy from ETC is not used to produce ATP and is instead dissipated as heat
In newborns, brown fat is present in interscapular, perinephric areas, and around the great vessels. Non-shivering thermogenesis can triple BMR in newborns.
Non-shivereing thermogenesis activation via β-receptors.
Endocrine response
Thyrotropin releasing hormone (TRH) is released.
- ↑TRH → ↑TSH → ↑T3/T4
- thyroid hormones increase metabolic activity in virtually all tissues, generating heat
Hunger
The hunger response is mediated by the hypothalamus in mild/early cold exposure.
The goal is to restore energy stores to maintain heat production.
Hunger may disappear in severe hypothermia due to impaired consciousness and slowing of metabolic processes.
Describe how thermoregulation is altered in a critically ill patient
Sedated, mechanically ventilated patients can lose 3-4°C if not actively warmed. Heat loss occurs through multiple pathways.
Airway
- Endotracheal tube exposes the airway to the environment → significant evaporative and convective heat loss
- Inspired gases must be actively heated and humidified to reduce further loss
Breathing
- Mechanical ventilation decreases work of breathing → less heat production
- Mandatory ventilation prevents autoregulation of respiratory rate and tidal volume
- hyperventilation increases evaporative and convective heat loss
Circulation
Vasodilators
- many drugs commonly used in ICU are vasodilators
- e.g. sedatives (propofol)
- e.g. vasoactivers (GTN, SNP)
- sedatives also blunt the normal vasoconstrictive response to cold exposure
- results in increased convective heat loss at the skin
Vasopressors
- decrease convective heat loss through the skin by causing cutaneous vasoconstriction (e.g. noradrenaline, vasopressin)
Inotropes
- augmentation of cardiac output increases cutaneous blood flow, increasing convective heat loss (e.g. milrinone)
Drugs
Sedation
- eliminates voluntary heat-preserving behaviours (seeking warmth, covering up)
- inhibits mechanisms that prevent heat loss
- circulatory effects as above
- inhibition of piloerection (goosebumps), which would otherwise trap warm air near the skin
- also inhibits mechanisms that increase heat loss (e.g. sweating), but this is not commonly an issue in ICU
- interthreshold range widens to 4°C (35-39°C)
- active heat production is inhibited within this range, preventing:
- shivering
- non-shivering thermogenesis
- endocrine response
- maximal vasoconstriction may not overcome heat loss by other mechanisms
- active heat production is inhibited within this range, preventing:
Paralysis
- prevents heat production due to voluntary and involuntary muscle activity
Metabolic rate may be altered by administration of some drugs
- e.g. thyroxine → ↑BMR → heat production
Environment
Convection
- critical care environments (ICU, operating theatre) are typically cool
- patients wear thin gowns and have limited blankets
- many patients have increased exposure to the environment due to:
- open abdomen or chest
- extracorporeal circuits (dialysis, ECMO)
- wounds or burns
- large bore surgical drains
Evaporation
- diaphoresis in critically ill patients increases evaporative heat loss
Conduction
- contact with cool surfaces (i.e. bed in ICU or operating theatre)
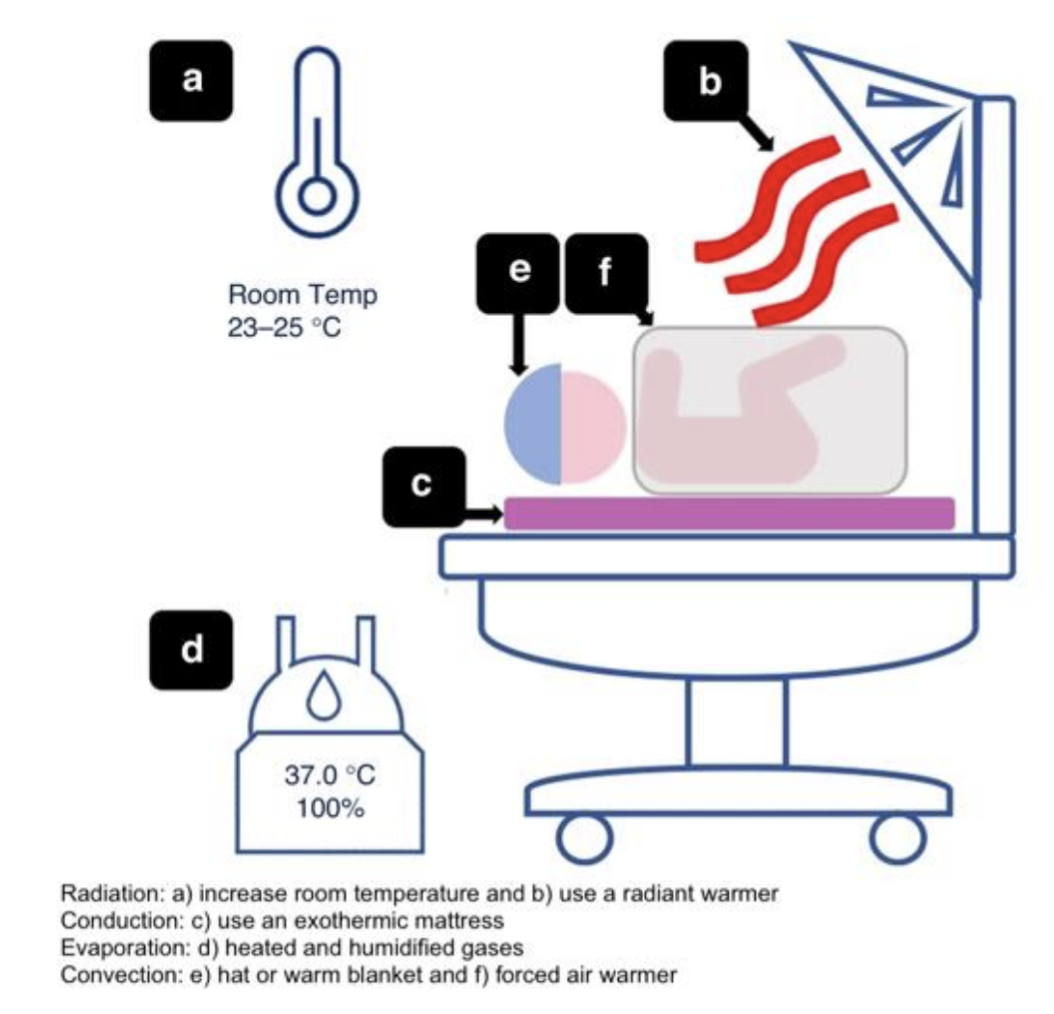
Heat loss minimisation in paediatric patients.
From Society for Pediatric Anaesthesia, CC-BY 4.0

